Decentralized Clinical Trials
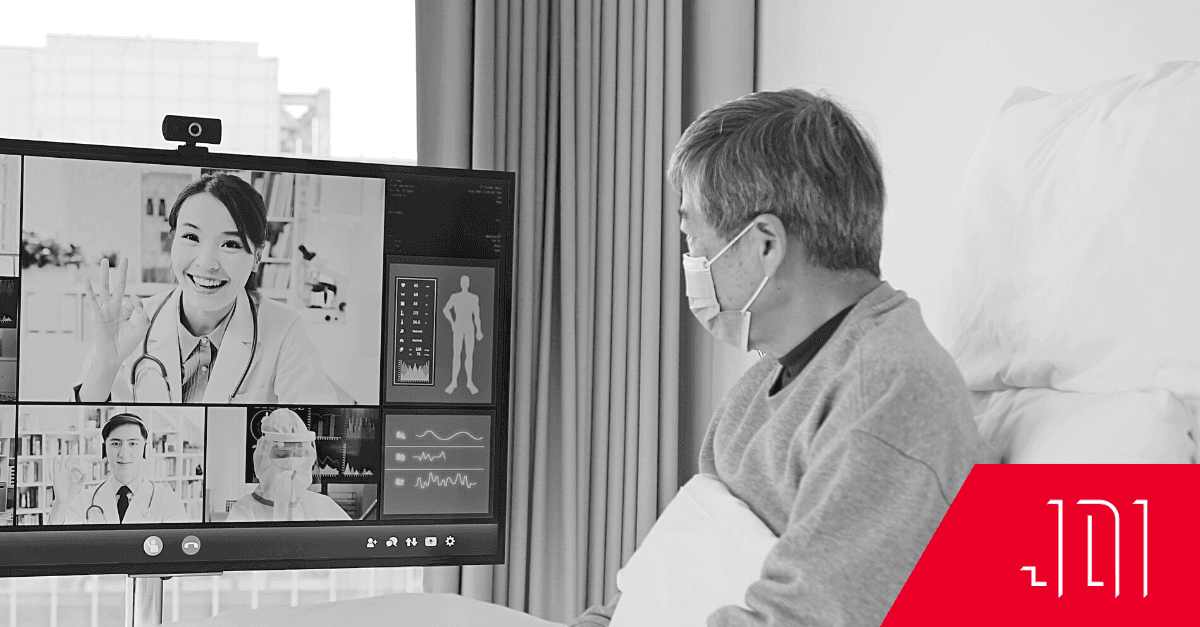
In May of 2023, the FDA issued its first guidelines concerning Decentralized Clinical Trials (DCTs) — a monumental step in creating better medical studies with stronger data. DCTs are a mix of telehealth and remote monitoring technologies that take a trial out of the clinic and into the real world. A trial can take place either completely remotely, or at a variety of locations convenient to the participant (local labs, clinics, or other healthcare facilities).
The need for decentralized clinical trials grew out of necessity during the first few years of the COVID-19 pandemic, and healthcare providers used the technology they could access. Now, DCTs show a promising way forward as the industry puts more trust in telehealth, wearable devices, and the security of health records and communication. The new models are so versatile and successful that over the last decade, all major pharmaceutical companies have conducted DCTs. In the future, drugs can be introduced into mainstream healthcare much more quickly than in decades past.
DCTs have a lot to offer the medical field, both in terms of better patient care and the acceleration of research. With the proliferation of telehealth services and the growing network of technology-savvy and well-connected healthcare providers, there are now many more options available for researchers who want to forge ahead.
How Do DCTs Fit Into The Provider Toolkit?
Like all patient care, DCTs are not one-size-fits all. One of the benefits of DCTs is that they can be customized and optimized for the best results. Some trials are completely virtual – best conducted using randomized data from patients wearing fitness trackers that collect heart rate, blood oxygen counts, and activity. After signing a consent form, these patients may never need to set foot inside a clinic – and yet their contributed data is vital to a clinical study.
Decentralized Hybrid Trials (DHTs) take place both in person and virtually. Many involve varying combinations of telehealth appointments, regular clinic visits, and home health care check-ins. They may involve wearable technology, mobile data collection, or in-person data checks. This flexibility in design creates a whole new world of opportunity for different types of research, and the reach of clinical trials is much further.
DCTs are not only much more flexible for the healthcare researchers, they help solve one of the most historically intractable problems in clinical research and drug development: access to diverse participants. DCTs and DHTs provide opportunities for researchers to reach new demographics, increase longer participation times, reduce patient burden, and collect crucial environmental data.
DCTs can significantly reduce barriers to patient participation. Sometimes travel is not possible for participants, or they live in rural areas where trial clinics are few and far between. To encourage the inclusion of rural or hard-to-reach participants, trial designers can enlist the help of local medical institutions, healthcare facilities, labs, and home health establishments. Patients might even be able to keep working with their local primary care physician, where trust has already been established.
DCT Technology
The rapid adoption of DCTs has only been possible because of new, easily accessible technologies. As of January, 2023, 91.8% of Americans had access to the internet in their homes. That’s up from 88% in just 2018. Along with access, both patients and providers are becoming more technologically savvy and comfortable using telemedicine for check-ins and remote monitoring.
The process starts with remote monitoring. The collection and use of real-time data through consumer wearable technologies like smartwatches and smart rings has become a common practice among athletes and health-conscious users. Many people voluntarily adopt these types of trackers for their own edification and self improvement, either to tweak their activity levels or to train toward personal goals. If the needs of a trial surpass the capabilities of consumer devices, there are a whole host of both general purpose and laser-focused devices that can be tailored to the necessary data points of a study.
Most importantly for researchers, the devices themselves are smaller, less expensive, and lack social stigmas that have plagued wearables in the past. Participants are more likely to engage with a trial and stay aligned on data collection, strengthening the findings of a study as a whole.
Even if trial participants aren’t used to wearables, a consumer device like a smartwatch makes setup and interfacing much more attractive.
It’s only a small jump to then send the data from the wearable to an Electronic Data Capture (EDC) system like Medidata or a real-world data capture system like Litmus Health, which allow for data to be collected with accuracy and efficiency. Medidata has been used for over 30,000 trials, and one of the founders of Litmus Health is helping to create and uphold DCT industry standards. Wearables are often targeted because they improve patient adherence, which brings down the cost of clinical trials. Once the data is collected, it’s sent to a Clinical Trial Management System (CTMS), which is a customizable software platform that project-manages everything from data analysis to payment processing to communication between providers and patients. Technology now streamlines the process to make trials faster, more accurate, and accessible to more people.
Practical Considerations
As the healthcare industry experiences a surge in successful research thanks to DCTs, support from outside the industry is making the transition from traditional to hybrid studies more feasible. DCTs depend on patient access to healthcare and insurance, dedicated infrastructure and staff, an adequate regulatory framework, and partnerships between research sites, patients and sponsors. Until a few years ago, many of these factors seemed like insurmountable obstacles.
People with no ability to travel due to disability, illness, or unreliable transportation have often been left out of important studies. As of 2019, 17% of people living in rural areas lacked internet access, compared to much higher rates in previous years. In 2021, Congress allocated $90B of ARPA and IIJA funds specifically for high speed internet access in rural and Tribal areas across the country, and the Rural Broadband Equity Project is working to ensure that the infrastructure for broadband access is sound. A more connected rural population means that people who ordinarily would not have access to clinical trials will soon become vital to clinical research.
New partnerships between research sites, patients, sponsors, and healthcare workers are also in the works. For instance, many trial sponsors seek help from clinical research organizations (CROs), which specialize in providing services to help facilitate research trials for sponsors. They can do anything from site selection and set up, to monitoring, to statistical analysis of reports and plans, creating seamless transactions for patients, doctors, and researchers all over the country.
People are ready. Clinical researchers have long known that patient-centric studies are more successful and accurate, and clinicians have begun to educate their patients about new studies and embed research into every day patient care. Plus, because there are so many fewer people involved across the board, DCTs are just faster and cheaper to conduct. This means there will be more trial opportunities for drug therapies and perhaps cures for rare diseases that some sponsors would deem too expensive for the return on investment if done by way of a traditional trial..
The Future of DCTs
It’s still early days for DCTs, so we can expect to see a lot of trial and error as the form develops. Some of the biggest issues are rooted in inconsistent data regulation and lack of best practices. The Clinical Research Data Sharing Alliance has been an industry leader in developing best practices for trial design and data protection, and with the help of the FDA, they’ve now set their sights on DCTs. The guidelines they create will help grow DCT models into flexible, scalable ones with the potential to reach millions of people who either wouldn’t qualify for clinical trials, or simply could not get to a clinic.
There’s work to be done, but it’s clear where the industry is heading, and the pace is accelerating as standards are adopted. DCTs are good news for patients, and they’re helping researchers reach more patients than ever before.